Pooling ICU facilities to improve care for Covid-19 patients
Cass operations expert has developed a new model which pools ICU facilities to improve care
Dr Navid Izady, an operations research expert at Cass Business School has developed a model which pools intensive care unit (ICU) facilities to improve care for Covid-19 patients. The model identifies the optimal subset of NHS trusts whose ICU capacity should be dedicated to Covid-19 patients so as to maximise the coverage of current virus hotspots, subject to moving non-Covid-19 patients no further than a certain distance away from their existing facilities.
Dr Izady explains his model, which he is happy to share with government and policymakers, below.
“The recent report produced by the Imperial College Covid-19 Response Team - ‘Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand’ - led to a substantial shift in the UK government’s policy in dealing with the virus.
“Simulating the growth of the epidemic and the impact of a range of interventions, the report concludes that under a suppression strategy, involving a combination of case isolation, general social distancing, and school and university closures, the peak intensive care unit (ICU) bed demand will fall below the capacity available (around eight beds per population of 100,000).
“The underlying assumptions of the report are that: 1) all ICU capacity in the country is accessible to all patients; and 2) all ICU capacity is dedicated to Covid-19 patients.
“Assumption 1, referred to as complete pooling of resources in the operations management literature, is not valid as patients in each area/region in the country have only access to ICU beds in their area/region. While it may be possible to transfer some patients to ICU facilities in other parts of the country, implementing this on a large scale is very challenging and certainly not cost-effective.
“Assumption 2 implies that there is no other patient requiring critical care in the hospitals which is not true. Thus, it is very likely that, even with a fully implemented suppression strategy, the NHS will have a (possibly large) shortage of beds in some facilities while spaces are available in some others.
“As such, to alleviate the situation described in the previous paragraph, changes must be made in the NHS current model of care delivery to achieve some degree of resource pooling without substantial cost.
“One strategy would be to dedicate the full ICU capacity of a certain subset of hospitals in the country entirely to Covid-19 patients. This would involve transferring the existing non-Covid-19 patients to neighbouring hospitals, but would enable the NHS to achieve some degree of resource pooling without significant cost.
“The higher economies of scale achieved under this model, as compared to the current model where Covid-19 patients are admitted to many ICUs along with other patients, would also facilitate provision and coordination of staff and equipment and thereby reduce the corresponding cost. Further, by allocating all beds in a facility to Covid-19 patients the variability in patients’ length of stay would decrease, resulting in a better service quality as suggested by queueing theory. Finally, this would reduce the chances of in-hospital transmission.
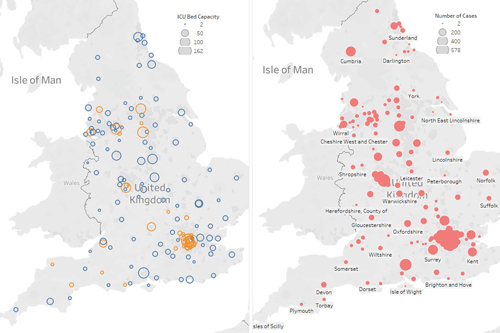
“I have developed a model to identify the optimal subset of NHS trusts whose ICU capacity should be dedicated to Covid-19 patients so as to maximise the coverage of current virus hotspots (based on published number of cases on 30th March 2020) subject to moving non-Covid-19 patients no further than 100 miles away from their existing facilities (based on end of January 2020 occupancy data).
“The model suggests that 38 of 141 NHS trusts’ ICU capacity should be dedicated to Covid-19 patients. This provides a fully dedicated ICU capacity of about 700 beds for these patients by moving about 600 patients to nearby hospitals.
“The location and size of the proposed dedicated facilities are highlighted in orange in the left panel in the graph below (other facilities are in blue). The right panel shows the spread of the virus.
“In this proposed delivery network, the newly developed Nightingale facility in London could act as an overflow facility, receiving patients from dedicated facilities in nearby hospitals once they become full. “
“The model could be re-run to include the recently hired private care facilities. It can also be run with estimates of case numbers at the peak of the pandemic (instead of the current spread) using the output from the Imperial model. The model can also be modified for finding the best location for other new facilities.”
Dr Navid Izady is a Senior Lecturer in Operations Research at Cass Business School. His research interests lie in stochastic modelling of service and manufacturing operations, in particular those relevant to healthcare. He is happy to be contacted to discuss this research.
